Adrenal Glands
The adrenal glands (Glandular adrenalis, ad-renalis) are two small, pyramidal hormonal glands, which are located on top of the kidneys. They are about 2 cm wide 4 cm long and thick and weigh about 5 - 10 g each. One main feature is their two-layer construction. They have a cortex and a medulla. Both have different functions and are therefore sometimes seen as two organs.
Adrenal medulla
The adrenal spinal cord is closely linked to the vegetative nervous system. It produces the two hormones adrenaline and norepinephrine, which are stored in vesicles within the marrow. If necessary, these stimulated the corresponding amount of hormones upon stimulation of the (sympathetic) nervous system. They have a stimulating effect and lead to an accelerated cardiac activity, increased blood pressure and a release of glucose so as to meet the increased energy requirements. The blood circulation of the muscles is also increased.
Adrenal cortex
The adrenal cortex accounts for about 75% of the total substance of the adrenal glands. This is due to the many different hormones that are formed in three different layers. These include mineral corticoids, glucocorticoids and sex hormones.
The most important hormone of the mineral corticoids is the aldosterone, which mainly acts on the kidney and helps to regulate the electrolyte and water balance. It promotes the reabsorption of sodium and helps retain water. Thus, it regulates the blood pressure and affects the blood volume. (In the case of an adrenal fatigue, this also explains the positive effect of drinking unrefined sea salt in water, because of the aldosterone deficiency it is difficult for the kidneys to retain sufficient sodium and water. The adrenal glands are then relieved of aldesterone production.)
The most important role of the glucocorticoids plays the cortisol and the cortisone. Both are indispensable to the body and control stress management. They affect carbohydrate, fat and protein metabolism. They are both stress relievers. In particular, they have a catabolic effect and build up proteins in muscles, fat tissue and the skin. They promote glucose synthesis in the liver, thereby increasing the blood glucose and causing the breakdown of fats to increase the content of fatty acids in the blood. In addition, they have anti-inflammatory effects and suppress an overwhelming immune reaction, e.g. for allergies.
The glucocorticoids are released in a circadian rhythm, ie they are subject to day-night (24h) fluctuations. Their release is controlled by the hypothalamus. It controls another region in the brain, the pituitary gland and regulates their activity. The pituitary gland then releases a certain amount of ACTH (adreno-cortico-tropic hormone), which in turn acts directly on the adrenal gland and causes it to release the stress hormones. In the morning, the highest cortisol level is to be measured, midnight the lowest value is reached. In stress situations the level normally also increases.
Another area of the Adrenal cortex is producing the male sexual hormones, the androgens. These include mainly testosterone and DHEA. Testosterone has an anabolic effect, it builds up proteins and affects the male sexual characteristics.
Stress Response
If the organism is exposed to a situation that it recognizes as a stress, ACTH is released by the hypophysis in a first reaction, which stimulates the adrenal glands to a stronger secretion of glucocorticoids (cortisol). In a second step, the sympathetic nervous system causes the release of adrenaline and norepinephrine (approximately 80:20). This reaction only works short term, so that the first mechanism prevails in long-term stress.
Stress is considered to be all situations that challenge the body. These include, for example, temperature fluctuations, cold, pain, injuries, surgeries, infections, low blood glucose, oxygen deficiency, emotions (joy, anger, anxiety, etc.). This includes activities which are fun such as e.g. parties . The body does not distinguish between good and bad stress.
up
Cortisol (The hormone of death)
The hormone with the outstanding importance is the cortisol, as it protects the body from excessive stress. It helps the organism to cope with stressors by:
- normalizing blood sugar. Together with the hormone insulin from the pancreas, cortisol regulates the blood glucose level. When the body needs more energy, cortisol engages and provides it. This enables an 'attack' or 'escape reaction' to master situations that threaten the organism. In people with adrenal fatigue, the cortisol level is initially high, but later, when the adrenal glands are exhausted, the cortisol production decreases and the blood glucose regulation becomes a problem.
- acting anti-inflammatory. Cortisol is a powerful drug against inflammatory reactions in the body. Small injuries, insect bites or e.g. joint injuries trigger an inflammatory reaction, the corresponding area swells, becomes red and warm. Cortisol keeps this reaction under control and ensures that the swelling does not become overwhelming and prevents excessive reactions, such as occur in allergies.
- acting immune-suppressive. A relatively weak immune system follows from a high cortisol level. It suppresses autoimmune reactions, as well as the cells of the own immune system, above all the white blood cells with their natural killer cells, monocytes, macrophages and mast cells.
- constricting vessels. Cortisol narrows medium-sized vessels. This results in low blood pressure in people with Adrenal Fatigue (later stages). They are less sensitive to other vasoconstrictors. High blood pressure, caused by magnesium and calcium processes is rather intensified.
- regulates stress. People who suffer from adrenal fatigue can not tolerate stress and their body is subject to the ongoing, strong stress. As the stress increases, the production of cortisol increases. If the adrenal glands can no longer meet the requirements, an adequate response is missing from the organism. Therefore, stress is fatal.
up
What Causes Adrenal Fatigue?
Stressors are the main cause of adrenal fatigue. Stress is different from person to person and often is not perceived as such. Frequent factors in the modern western world are working conditions, death of a loved one, change of location, job change, illness, injury, divorces, environmental toxins, etc. If the body can no longer compensate for stress, Adrenal Fatigue develops. Circumstances which may contribute to:
|
|
Some conditions are not recognized correctly, since especially chronic infections can be subclinical and show no symptoms. Frequent and severe stressors are chronic inflammation caused by bacterial and parasitic infections such as H. pylori or Giardia. In the case of strong forms, the spine should always be checked.
up
How chronic stress affects the body
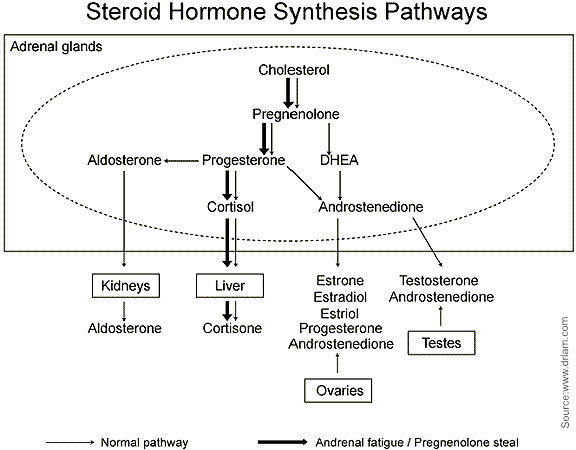
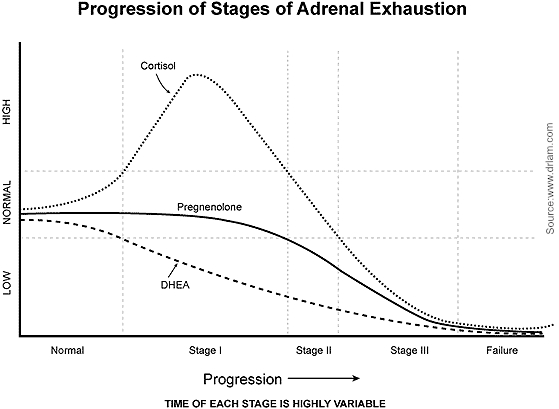
As mentioned earlier, stress stimulates the release of the hormone ACTH via the sympathetic nervous system and thus stimulates the adrenal glands to an increased production of cortisol. Significant chronic stress can cause the adrenal glands to deplete and the amount of cortisol produced decreases. The level of DHEA (a hormone that is also formed in the adrenal gland) decreases without first advancing. This initially results in an increased ratio of cortisol to DHEA.
The hormones are subject to a control system with negative feedback. This ensures that an adequate amount of hormones is always available. If the concentration in the blood is too high, the delivery is not further amplified but instead throttled. Thus, a high cortisol level is normally registered by the brain and the hypothalamus subsequently reduces the output of ACTH, thus reducing the further production of the hormone in the adrenal glands.
In case of severe chronic stress leading to adrenal fatigue, this mechanism is broken. The high cortisol level is registered but the body interprets this as a persistently menacing situation and keeps the production constant or even increases the cortisol in order to manage the danger and to ensure its own survival. There is no decrease in cortisol production as long as the risk (stress) persists. The negative feedback is bypassed and the body reacts in the opposite direction. Cortisol as (anti-) stress hormone means danger and to counter this it is produced more. If this condition persists long enough, the adrenal glands are no longer able to recover and exhaust themselves with time. You can no longer provide enough hormones throughout the day. This can be measured with a cortisol day profile, which can be obtained from saliva samples.
This situation does not remain without consequences. The initial high ratio between cortisol and DHEA can lead to a reduced insulin sensitivity of the body which leads to increased blood glucose levels and diabetes. In addition, the synthesis of an important immunomodulator IgA as well as of natural killer cells and T-lymphocytes decreases. This results in a weakened defenses and infections such as herpes, Candida albicans or viral infections can more easily take hold. In addition, the calcium intake can be disturbed and an increased protein degradation can lead to muscle weakness. Increased water and salt resorption can lead to increased blood pressure in this phase and estrogen dominance is possible, which can lead to PMS ailments among women.
up
How does Adrenal Fatigue develop? Phases of the disease.
Phase 1, alarm reaction:
In this phase, the body reacts aggressively to the existing stressor. There is an escape or fighting situation in which the body increases the production of cortisol. For this purpose, the output of ACTH from the hypophysis is increased. DHEA decreases as the organism tries to overcome the danger. To this end, the adrenal medulla is strongly stimulated to release adrenaline. If the stress persists for a long time, the adrenal gland is no longer able to meet the high demands of the body.
Phase 2., persistent reaction:
If chronic and severe stress persists, the adrenal glands begin to deplete. They can no longer cover the strong demand for cortisol and consequently its level drops. From a high level, the level drops back towards normal while the ACTH remains high to further stimulate the adrenal glands. Usually the cortisol level is lowered in the morning, noon and afternoon, but usually normal at night.
At this time, a "pregnenolone-shunt" may occur. Through this phenomenon, the metabolic pathway (see above) in the adrenal glands is increasingly used for the production of the cortisol. Other hormones such as the estrogen, testosterone or DHEA are hardly formed yet. The body ties to get as much cortisol as possible. As a result, the cortisol level remains unchanged, while pregnenolone production decreases. Now the cortisol level in the morning is clearly too low, but at night usually still sufficient.
Phase 3. Exhaustion:
In this phase, ACTH is elevated, cortisol decreased, and DHEA is far below the average. This stage can develop over the years. The organism is now no longer able to produce a sufficient quantity of cortisol and to cover the needs. Even at night, the cortisol level is low and the stress axis (hypothalamus-pituitary-adrenal gland) fails, so the body gets out of balance. Frequently severe imbalances of the sex hormones such as estrogen, progesterone and androgens occur and announce an adrenal failure.
Phase 4, Failure:
Now the adrenal glands are completely exhausted. In this phase, there is an increased risk of circulatory failure and death.
Why is Adrenal fatigue overlooked?
Although a subclinical adrenia (adrenal subfunction) has been known since the beginning of the last century, it is overlooked by school medicine. This is mainly due to the fact that it is extremely difficult to prove this by means of the standard blood tests. These tests show only an absolute, severe deficiency of adrenal hormones to which is known as Addison's disease. This disease is very rare, as is Cushing's disease, in which excessive adrenal hormones are produced.
In adrenal fatigue, they are low-level adrenal hormones but still in the normal range and often too high to clearly diagnose a Addsion's disease. So our hormones can only be half the optimal, but still as normal. These "normal" blood values do not mean that you are free of Adrenal Fatigue!
Conventional physicians are not trained to detect subclinical adrenal fatigue. They do not know the significance of subclinical adrenal fatigue because they have not learned it. They are misled by the normal blood tests, which are not sensitive enough to indicate Adrenal Fatigue. As a result, patients who are tested for their adrenal function are considered healthy, although their adrenal glands work suboptimally. They show clear signs and symptoms that their bodies urgently need help and attention.
up
Thyroid Gland
The thyroid gland (Glandular thyreoidea) is a hormonal gland which is located in the human body below the larynx in front of the air tube and has a butterfly-like shape. It is placed underneath the thyroid cartilage and lies in the shape of a shield around the annular cartilages of the larynx.
The thyroid gland consists of two lobes, which are connected to each other in the middle and form a H as a whole. It can be as heavy as 60 g (even without a pathological value), but weighs usually between 18 and 25 g for a length of about 3-5 cm.
The main function of the thyroid is the secretion of various hormones and iodine storage. Central hormones such as thyroxine (tetraiodothyronine, T4) and triiodothyronine (T3) are formed here as well as the peptide hormone calcitonin. Its opponent, on the other hand, the parathormon is formed in the parathyroid glands.
T4 and T3 are stored (also formed) in folipid thyroid glands and released as required. They regulate the energy conversion of the body. The calcitonin and the parathormone are involved in the metabolism of the calcium metabolism and affect bone formation and breakdown.
Thyroxine and triiodothyronine
The hormones T4 and T3 are both formed by the thyroid gland upon stimulation of the pituitary gland. The brain pituitary gland controls thyroid hormone activity via the TSH (thyroid stimulating hormone) and is itself controlled by another brain region, the hypothalamus, via the TRH (thyreotrophin realeasing hormone). The most potent (about 100x) more active hormone is the T3, which can be formed by the elimination of an iodine atom from the larger thyroxine (T4). This is done according to the needs of the organism. At the same time, a certain amount of Reverse-T3 (RT3) is also formed, but this is physiologically ineffective. The amount of T3 and T4 has a negative feedback on the pituitary and the TSH and thus ensures a constant hormone level.
In the cell nuclei of the target cells the T3 acts on basic metabolic processes of the body. It acts stimulating and
- Increases heart rate and blood pressure
- Increases carbohydrate, fat and connective tissue metabolism
- Stimulates the activity of the sweat and sebaceous glands
- Boosts bowel motility
- Promotes heat development (energy consumption and basic turnover are increased)
- Increases oxygen consumption
- Increases glucose formation and releases glycogen from the liver
- Activates the turnover of body fat deposits and accelerates the cholesterol metabolism
- Affects water retention and bone formation
- Affects the development of the skeleton and the maturation process of the brain
up
Interactions
The thyroid gland and the adrenal gland also influence each other, which is often ignored. This is sometimes followed by poorly adjusted 'hypothyroidism', which may show little progress under therapy.
One could say that the thyroid gland 'provides' and 'regulates' the energy of the body (via T3 and T4) but the adrenal glands must be strong enough to cope with this metabolic energy. A strongly increased metabolic activity is interpreted by the adrenal glands as stress, they have to function optimally in order to manage the metabolic energy. If, therefore, the concentration of T4 and / or T3 is increased with a hormone substitution, the adrenal glands must be capable of adapting to this situation. However, this is not always the case. If they are too weak and produce too small amounts of cortisol, they will be overloaded and try to lower the thyroid gland by providing the pituitary less TSH. This may result in a return to the symptoms after the initial improvement, or (with a continuous increase in the dose), the adrenal glands deplete and a state of low energy arises.
If both organs are affected, the adrenal glands should always be strengthened first before treatment of the thyroid gland. In weak adrenal glands, normal thyroid activity may be too great a burden. It can happen that in a hypoadrenal state (coldness, weight loss, sleep disorders, anxiety, exhaustion, dry skin) the activity of the thyroid gland is reduced by increasing RT3. On the other hand, if the thyroid gland is too weak to keep up with the adrenal glands, you may begin to feel 'hypothyroid' (heat sensitivity, weight gain, fatigue, increased sleep needs and / or depression). It is usually a mixed form, so that one can focus not only on one organ.
